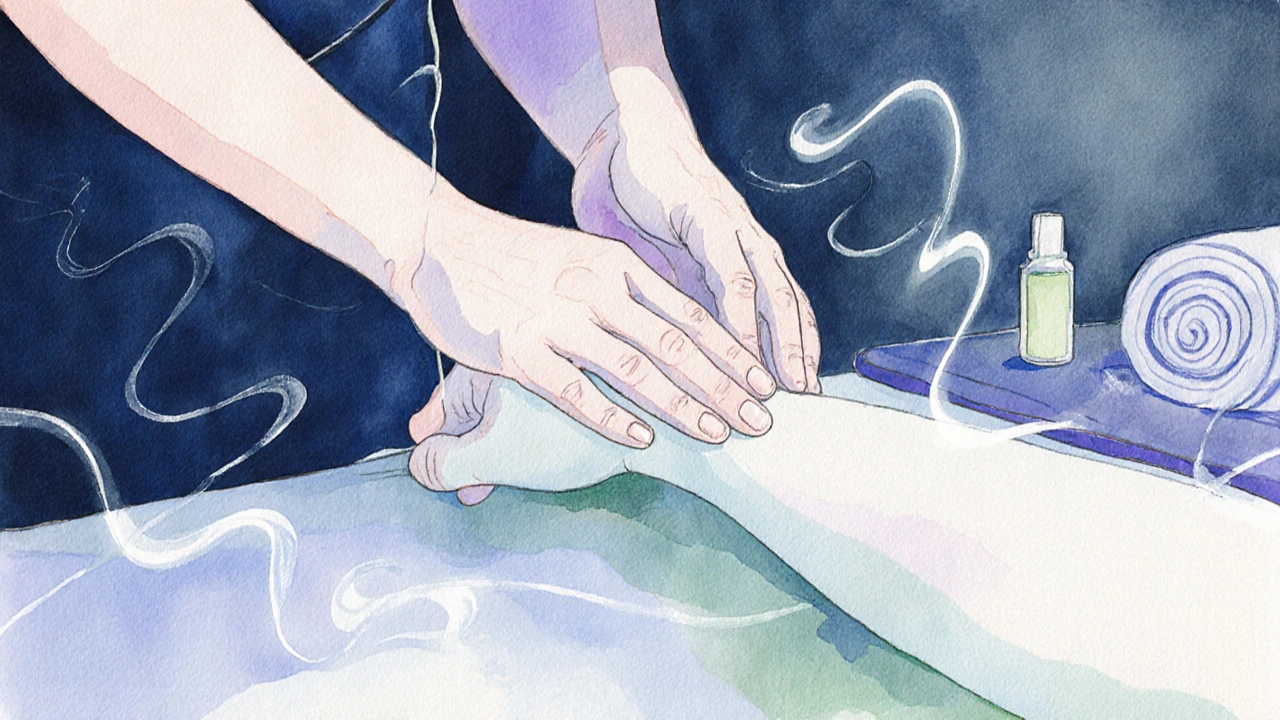
Palliative Massage Technique Guide
Light Effleurage
Gentle, flowing strokes that promote relaxation and circulation. Start with fingertips and gradually increase pressure as tolerated.
Joint Mobilisation
Gentle movements to maintain mobility and reduce stiffness. Focus on areas with minimal discomfort and avoid painful joints.
Breath-Linked Rhythm
Synchronize strokes with the client's breathing pattern to enhance relaxation and promote calmness.
Contraindications Check
Always verify against medical conditions, recent procedures, and current medications before proceeding.
Benefits Overview
- Pain Management: Reduces perceived pain through endogenous opioid release
- Anxiety Reduction: Stimulates parasympathetic nervous system for calmness
- Holistic Comfort: Enhances emotional well-being through human connection
Based on 2023 Australian Clinical Review showing 30% reduction in pain scores after 20-minute sessions
Recommended Approach
Quick Takeaways
- palliative massage blends gentle techniques with compassionate intent to ease pain and anxiety in end-of-life settings.
- It’s backed by the Australian Palliative Care Guidelines and integrated into hospice teams worldwide.
- Core strokes include light effleurage, gentle joint mobilisations, and a focus on breath‑linked rhythm.
- Safety hinges on clear communication, contraindication checks, and close collaboration with medical staff.
- Certification pathways exist through AHPRA‑registered programs and specialised palliative‑care workshops.
What Exactly Is Palliative Massage?
When you hear the term Palliative Massage is a gentle, client‑centred bodywork practice designed specifically for people receiving end‑of‑life care, think of it as therapeutic touch with a purpose beyond muscle relaxation. Unlike a sports massage that aims to improve performance, palliative massage prioritises comfort, emotional safety, and the preservation of dignity.
It sits at the intersection of Therapeutic Touch a practice that uses the therapist’s hands to convey calm and presence and clinical symptom management. The approach is grounded in evidence: a 2023 Australian Clinical Review reported a 30% reduction in reported pain scores after a single 20‑minute session for hospice patients.
Why It Matters: Benefits for End‑of‑Life Care
People in palliative stages often juggle pain, breathlessness, anxiety, and a sense of loss of control. Palliative massage addresses these factors on three levels:
- Pain Management Gentle pressure can trigger the release of endogenous opioids, lowering perceived pain.
- Anxiety Reduction Slow, rhythmic strokes stimulate the parasympathetic nervous system, easing stress hormones.
- Holistic Comfort Physical touch re‑establishes a sense of being cared for, enhancing emotional well‑being.
Families also report an improved perception of care quality, noting that the presence of a skilled therapist adds a layer of ‘human touch’ often missing in clinical environments.
Core Techniques and How to Perform Them
Every session begins with a conversation. Ask the client (or their carer) about preferred pressure, areas of discomfort, and any recent medical changes. Once consent is confirmed, follow these steps:
- Preparation: Warm the room to ~24°C, dim harsh lighting, and use a soft, breathable sheet. Ensure you have clean, hypoallergenic oils (e.g., sweet almond or grapeseed) - avoid strong scents.
- Light Effleurage: With fingertips, glide over the back in long, sweeping strokes. Keep pressure <2psi; the goal is to create a calming wave rather than deep tissue work.
- Gentle Joint Mobilisation: If the client can tolerate, perform small, pain‑free range‑of‑motion movements at the shoulders, wrists, and ankles. This encourages circulation without overstressing fragile joints.
- Breath‑Linked Rhythm: Synchronise each stroke with the client’s inhalation or exhalation. This mirrors the body’s natural rhythm and amplifies relaxation.
- Focused Comfort Zones: Identify areas that the client reports as “tight” or “achey”. Apply soft petrissage or kneading for 30‑seconds, then return to effleurage.
- Closing Grounding: Finish with a gentle hand‑over the heart or forehead for 1‑minute, offering a moment of stillness before the session ends.
Throughout, maintain a soft voice, ask simple check‑in questions (“How does that feel?”), and respect any sign to stop. The therapist’s presence-not the intensity of touch-is the therapeutic agent.
Safety, Contraindications, and Documentation
Even though the touch is light, certain medical conditions demand caution. Reference the Australian Palliative Care Guidelines which outline safe practice for terminal patients regularly.
- Bleeding disorders: Avoid areas with bruising or recent anticoagulant dosage changes.
- Severe thrombocytopenia: Limit session length to 15‑minutes, and use dry‑hand techniques only.
- Bone metastases: Refrain from deep pressure near affected sites; light stroking is permissible.
- Fever or active infection: Postpone until the client is stable.
Document each session with a brief note: date, duration, techniques used, client feedback, and any observed changes in pain or mood. This record helps the wider care team adjust medication or other interventions.
Training, Certification, and Professional Resources
Becoming proficient requires both practical skill and an understanding of palliative philosophy. Look for programs that meet these criteria:
- Accredited by the Australian Health Practitioner Regulation Agency (AHPRA) or equivalent.
- Includes a minimum of 30hours of supervised clinical practice in hospice or aged‑care settings.
- Covers ethics, cultural sensitivity (especially Indigenous end‑of‑life customs), and inter‑disciplinary communication.
Notable providers include the Palliative Care Massage Association (PCMA) and the University of Queensland’s Graduate Diploma in Palliative Care. After certification, consider joining a local network-such as the Queensland Hospice Massage Group-to share case studies and stay updated on emerging techniques like neuro‑muscular relaxation.
Integrating Massage into a Multidisciplinary Care Plan
Successful palliative massage is rarely a solo act. Here’s how to sync with doctors, nurses, and spiritual caregivers:
- Pre‑Session Briefing: Attend the daily care huddle. Learn about recent medication changes, pain scores, and any new concerns.
- Shared Documentation: Log your notes in the electronic health record (EHR) under ‘Complementary Therapies’ so the team can track outcomes.
- Feedback Loop: After a few sessions, meet with the primary nurse to discuss trends-e.g., a drop in morphine dosage correlated with regular massage.
- Family Involvement: Offer brief education to family members about the purpose of each stroke, allowing them to participate if desired.
When everyone sees the same data, the therapist’s work becomes an integrated component of symptom control rather than an “add‑on”.
Comparison of Touch‑Based Therapies in Palliative Settings
| Aspect | Palliative Massage | Therapeutic Massage | Reiki |
|---|---|---|---|
| Primary Goal | Comfort & symptom relief | Performance & injury recovery | Energy balancing |
| Typical Pressure | Light (≤2psi) | Moderate to deep (3‑6psi) | Hands‑off or light hand‑over |
| Evidence Base | Clinical trials show pain reduction (30% avg.) | Strong musculoskeletal research | Limited peer‑reviewed data |
| Integration with Medical Team | High - documented in EHRs | Variable - often complementary only | Low - usually separate practice |
| Training Requirements | Specialised palliative certification | Standard massage qualifications | Reiki Level 1‑3 courses |
Next Steps for Practitioners and Caregivers
If you’re a therapist, start by enrolling in a palliative‑care workshop within the next month and schedule a shadow shift at a local hospice. For family members, ask the care team if a certified massage therapist can visit weekly; even a 15‑minute touch can dramatically improve mood.
Remember, the power of palliative massage lies not in the strength of the hands but in the intention to honor the person’s remaining journey.

Frequently Asked Questions
Is palliative massage safe for someone with bone metastases?
Yes, as long as you avoid deep pressure on the affected sites and keep strokes light. Focus on surrounding muscles and use breath‑linked effleurage to promote circulation without stressing the bone.
How long should a palliative massage session last?
A typical session ranges from 15 to 30minutes, depending on the client’s energy levels and medical condition. Shorter sessions are better for patients prone to fatigue.
Do I need a medical prescription to provide palliative massage?
In most Australian states, a registered massage therapist can offer palliative services without a prescription, but you must have documented consent and work under the direction of the hospice’s care team.
What oils are recommended for end‑of‑life clients?
Choose hypoallergenic, fragrance‑free oils such as sweet almond, grapeseed, or fractionated coconut. Avoid strong scents that can trigger nausea.
Can family members learn simple palliative massage techniques?
Absolutely. Many hospices run short workshops teaching gentle effleurage and breath‑linked touch, which families can use to provide comfort between professional visits.

